Pancreas and the disorders associated with it

What is the Pancreas and the disorders associated with it?
The pancreas was largely ignored in the past – both as an organ as well as a seat of the disease. It was only in the 17th century that the pancreatic anatomy was discovered and its significance in disease was demonstrated. Even then, its role in digestion was not known. Claude Bernard discovered the function of the pancreas in digestion and later, in 1922, Banting and Best discovered insulin from the pancreatic cells. Over the years, we have been able to understand a lot more about the functioning of the pancreas and its importance in digestion and maintaining body functions.
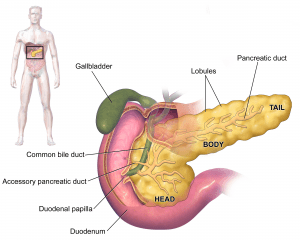
The pancreas can be found in the abdomen. It is a gland organ and a component of the digestive system that creates insulin as well as other vital enzymes and hormones that aid in the digestion of food. The pancreas performs an endocrine role by releasing hormones(principally, insulin) directly into the bloodstream, as well as an exocrine function (Required for digestion) by releasing molecules called enzymes into the intestine via the pancreatic duct. The pancreas secretes enzymes, or digestive juices, into the small intestine which helps in breaking down the food that is consumed and gets passed from the stomach into the intestine.
The pancreas also produces and secretes the hormone insulin. This hormone regulates the body’s glucose or sugar levels in the bloodstream. Disorders of insulin secretion can result in Diabetes and other related diseases. Pancreatitis and pancreatic cancer are two other potential health issues commonly encountered and related to the pancreas.
Because the pancreas is inaccessible, diagnosing pancreatic disorders can be difficult. There are several ways to assess pancreatic function. A detailed history and physical examination is the first step of any evaluation that can suggest pancreatic disorders through specific signs and symptoms such as – typical abdominal pain(upper abdomen, boring type of pain radiating to the back, which gets aggravated on lying down and with food intake), vomiting, increased heart rate, and upper abdominal tenderness. However, these symptoms are not specific and require further evaluation to identify pancreatic diseases. Blood tests are the next step which can indicate the presence of pancreatic disorders.
The Ultrasound abdomen, CT (computed tomography) scan, endoscopic ultrasound, and MRI are various imaging modalities used for evaluating pancreatic diseases. Among these, an ultrasound abdomen is the first step that can indicate pancreatic inflammation. Definitive diagnosis is usually achieved by a CT scan of the abdomen/MRI abdomen. Specific sequences of these scans are required for accurate visualization of the pancreas and it is recommended to undergo these scans at tertiary care centers with experience in handling patients with pancreatic disorders. Endoscopic ultrasonography is a relatively new modality that is used for the accurate delineation of the pancreas and provides excellent information on the pathological processes in the pancreas. However, EUS experience and proficiency are not common and are usually limited to tertiary care centers with a high load of patients with pancreatic illnesses. ERCP (endoscopic retrograde cholangiopancreatography) and MRCP are two tests used to assess the pancreatic ducts (magnetic resonance cholangiopancreatography).
Symptoms of pancreatic malfunction
The pancreas has multiple functions. It produces hormones like insulin required for glucose regulation in the body. It also produces enzymes that help you digest meals and absorb nutrients. You’re likely to have at least some of the following symptoms if your pancreas isn’t working properly:
Tenderness, swelling, or recurrent pain in the abdomen; nausea or vomiting; excessive gas formation, diarrhoea / oily malodorous stools, unexplained weight loss and malnourishment, and inability to tolerate fried food.
What are some pancreatic disorders?
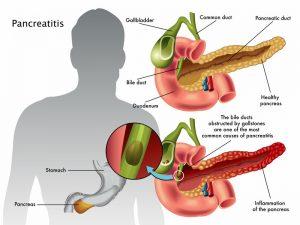
Acute Pancreatitis
Acute pancreatitis refers to inflammation of the pancreas that occurs suddenly and is frequently accompanied by significant intermittent upper abdominal pain that can be prolonged for several days. The pain is severe and radiates to the back, aggravated by food intake and lying down. It can be associated with nausea, vomiting, abdominal distension, and in severe cases, can have low blood pressure and altered consciousness. Common causes of acute pancreatitis include alcohol intake, stones in the gall bladder, certain genetic disorders, and even a few drugs that have been known to cause acute pancreatitis.
Chronic alcohol use is an especially common cause of acute pancreatitis. Not all patients who consume alcohol get pancreatitis, but it can cause significant pancreatic damage and lead to chronic pancreatitis (permanent dysfunction of the pancreas) in the future. Treatment of acute pancreatitis is largely supportive and measures to give the pancreas some rest in order to heal. The majority of people who have acute pancreatitis show a full recovery. However, a proportion of patients require long-term follow-up in high-risk clinics for pancreas in order to look for early changes of chronic pancreatitis which will necessitate a different line of management.
Chronic Pancreatitis
Chronic pancreatitis is a disease that causes permanent damage to the pancreas resulting in progressive deterioration of pancreatic function over time. It is more commonly seen among males between the ages of 30 and 40 years. Chronic pancreatitis may present with an acute episode of pancreatitis at first and might be mistaken for acute pancreatitis because the symptoms are similar. This is why a thorough evaluation by an expert in pancreatic disorders is essential in all patients of acute pancreatitis in order to diagnose chronic changes early. In the long term patients with chronic pancreatitis can have weight loss, oily stools, diabetes with poorly controlled sugars, malnutrition with vitamin deficiency, and chronic abdominal pain. The most dreaded complication of chronic pancreatitis is pancreatic cancer which can be insidious in onset and usually diagnosed late. This is why all patients of chronic pancreatitis require regular medical checkups with an expert in pancreatic diseases in order to screen for malignancies. There are a few centers where high-risk screening clinics are available to cater to patients with chronic pancreatitis. However, this is only just evolving and is not widely available yet.
Hereditary Pancreatitis
Pancreatitis is sometimes linked to genetic disorders. Patients with specific genetic mutations affecting pancreatic function can present early in life (before age 30), and acute recurrent pancreatitis typically evolves into chronic pancreatitis on follow-up. Cystic fibrosis is the most frequent genetic condition that leads to chronic pancreatitis. According to new research, genetic testing can be a useful tool for identifying patients who are predisposed to hereditary pancreatitis. These tests are usually done in conjunction with pancreas clinics and with the recommendation of experts experienced in handling pancreatic diseases.
Hereditary pancreatitis, like chronic pancreatitis, is a progressive condition with a significant risk of long-term complications. Chronic abdominal pain, diarrhea, malnutrition, and diabetes are all possible sequelae in the long term. Pain management and long-term pancreatic enzyme replacement are the mainstays of treatment.
Pancreatic Cancer
Pancreatic cancer accounts for the fourth-highest number of cancer-related deaths among males and the fifth-highest number of cancer-related deaths among females. Pancreatic cancer has earned notoriety as cancer with poor response to therapy and poor outcomes. It has a propensity to spread to distant organs and is usually diagnosed later than most other forms of cancer. This is mainly due to little to no symptoms in the early stage of the disease. Once the tumor spreads to the bile duct and neighboring structures, patients can present jaundice which is, a yellowish discoloration of skin, eyes, and mucous membranes. In addition, patients can present with gastrointestinal bleeding, abdominal pain, loss of weight, and appetite. Diagnosis of pancreatic cancer rests mainly on blood tests and imaging modalities. Among imaging modalities, a CT abdomen with a specific contrast protocol or an MRI abdomen can be extremely useful in identifying the tumor in the pancreas. In the past, getting a tissue diagnosis via biopsy was extremely challenging in patients with pancreatic cancer owing to the location of the organ which makes access difficult. However, with the advent of Endoscopic ultrasound (EUS), the pancreas can easily be assessed and a fine needle biopsy can be performed which has been shown to be safe and reliable.
In the early stages, pancreatic cancer can potentially be cured with surgical excision in combination with chemotherapy. Newer immunotherapy options have also shown promising results. However, most patients present at later stages of the disease which precludes surgery. At this stage, palliative treatment options include chemotherapy, ERCP with the placement of stents (metal tubes that keep the bile duct patent), and supportive therapy. Early diagnosis of pancreatic cancer is hugely beneficial and needs more attention. Screening for pancreatic cancer in high-risk groups like chronic pancreatitis and patients with hereditary pancreatitis could be beneficial. The provision of high-risk screening clinics for pancreatic cancer has been started in the west and needs to be encouraged in India.
If you have intermittent mild abdominal pain with bloating occasionally of short duration, it may not be necessary to visit your doctor. However, if you experience recurrent digestive problems, it could indicate a serious underlying disorder and it’s critical to identify and diagnose early so that you can begin treatment.
It would be advisable to seek medical attention in case of symptoms like recurrent abdominal pain, foul-smelling oily stools, unintentional weight loss, and loss of appetite. In addition, known diabetic patients with worsening sugars could also be harboring a pancreatic tumor and need evaluation. Pancreatic disorders often have vague symptoms and a trained medical expert would be able to suspect and evaluate for such red flag signs early so as to ensure early diagnosis of treatment of these conditions. In the case of pancreatic diseases, prevention, and early diagnosis is always better than the elusive cure.
Dr. HARSHAVARDHAN RAO B
Medical Gastroenterology
Professor/ Senior Consultant
MD. DM Gastroenterology


