Migrating Foreign Body Pellet
A 38-year-old female presented to the emergency department with an alleged history of penetration of air borne metal piece into the right side of the neck. She was standing near welding work at around 3:30 PM on 07/01/2021 and sustained neck injury. Followed by which she had a severe piercing pain in the neck and complaints of Difficulty and painful swallowing.
On Inspection there was a small entry wound was noted on the right side of the neck measuring 1 x 1 cm, 2 cm from the mid line, 4 cm from the anterior border of the sternocleidomastoid, 4 cm from hyoid and 6 cm from the clavicle. The skin over the wound is oedematous and erythematous. Exit wound was not found.
On Palpation Tenderness was present around the entry. No subcutaneous emphysema or neck swelling was noted. No foreign body was visible or palpable in the neck.
Further she was evaluated with x-ray of the neck, it showed a radio opaque foreign body in the prevertebral region opposite to the C7 vertebral body.(Fig.1)

Patient was taken up for Emergency Neck exploration under general anaesthesia. Patient was positioned. Parts painted and draped. Incision was taken around the entry wound ( Fig.2).

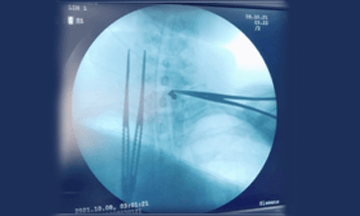
Subcutaneous and strap muscles were dissected. Dissection was done on right side of the trachea till the vertebra and a foreign body could not be visualized or felt. Hence the procedure was abandoned. Next day, CECT neck was done on the next day to relocate the foreign body, it was found to be near the trachea-oesophageal groove. So re-exploration of neck was done. Incision extended to the opposite side. This time dissection was done on the left side, medial to the sternocleidomastoid muscle and carotid sheath was retracted and dissection was done till the C7 vertebra. With the help of the C – arm the foreign was identified (Fig.3).
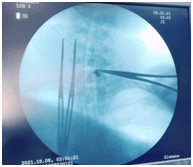
A hard substance was felt in the muscular layer of the posterior part of the oesophagus below the cricoid at the C7 level without opening the lumen of the oesophagus, after fixing it with forceps the foreign body was removed in toto (Fig.4) carefully without damaging the mucosal layer of oesophagus.

Postoperatively patient was on intravenous antibiotics. She was kept in NPO for 1 day followed by Ryle tube feeds. Oral test feeds was given on POD7. Drain removal was done on POD 7. The patient was taking orally well. Ryles tube was removed. The post-operative period was uneventful.
Horizontally-oriented foreign bodies are more likely to penetrate the oesophageal lumen. Mechanisms include strong oesophageal peristaltic movements against the foreign body, neck movement, and careless manipulation of the foreign body while attempting to remove it may influence the risk of perforation. A bullet can gradually move in soft tissue adjacent to the entry wound, penetrate to other organs and pass even about half body length without any symptoms, until it causes obstructive or compressive effects or impacts vital organs. 4 To recognize the direction of the bullet among shooting victims, immediate exploration of entry and exit wounds is necessary.
A high index of suspicion is needed to diagnose a type of migrating foreign body, as patient might not be aware of the cause of an injury as in our case.
Complete detail history and early surgical intervention is crucial in such cases to prevent fatal complications.
Though there was a migrating foreign body, successful removal was achieved with the help of intraoperative radiography and timely decision in our case.
DR. HARSHAVARDHAN N. REDDY
Ear, Nose & Throat (ENT)
Consultant
MBBS, MS ENT

