The Silent thief of sight
Do you know who this is? It’s the one that raises your eye pressure, snuffs out your optic nerve, and reduces your field of view. And his name is Glaucoma. From the epiglottis. He navigates your eye in a sinister fashion. We don’t even know all his details. Like Don. Don ko pakadna mushkil hi nahin, Namumkin hai. He catches you unawares when most of the damage is done. And he does not just leave with you, he can trouble your family as well.
But, you know what the good news is? We can keep him at bay. Catch the signs early, just the way we use CCTV cameras to keep our houses and offices safe. Who is better than the ophthalmologists at Ramaiah Hospital to do this job?
So how do we keep an “eye” on glaucoma? We do a routine check on all people over the age of 40. This is more so when there is a family history of glaucoma. How do we examine this? We check your eye pressure. We do this using a tonometer, which checks your intraocular pressure. Then, we check your visual field using Humphrey’s Visual Field Analyser. Further, we check your optic nerves to see whether any damage is done.
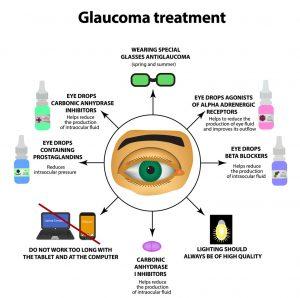
Life is like a box of chocolates, you never what you are gonna get. We catch the problematic one, and we decide how best we can treat the problem. there are various ways. Sometimes, just a regular check is all that you need. Others would need eyedrops that have to be used on a daily basis. Some others require lasers to treat the issue. A few others might require surgery that helps drain out the excess fluid in the eye, so as to maintain eye pressure. We call it a trabeculectomy.
Your eyes. They toil day in and day out for you, untiring, whether sun or rain. So give your beautiful eyes the love they need. Get them checked. Have glaucoma ruled out? Don’t #feelthe pressure!
FAQs:
-
What is Glaucoma?
Glaucoma refers to a group of diseases that damage the optic nerve, which carries visual information from the back of the eye to the brain. Risk factors for glaucoma include age, family history, the shape of the eye, race/ethnicity, and increased eye pressure. Although glaucoma may not have symptoms in the beginning, eventually permanent vision loss can occur.
-
How Does Eye Pressure Affect Glaucoma?
Elevated eye pressure increases the risk of having glaucoma. However, it is also possible to have glaucoma with average or below-average eye pressure (often termed normal tension glaucoma). Therefore, eye pressure is one of the ‘vital signs’ of a glaucoma check-up but does not define glaucoma. Decreasing eye pressure is the only way we currently know to decrease the onset or progression of glaucoma-related vision damage. Therefore, the treatments for glaucoma, including medications, lasers, and surgeries, all work towards lowering eye pressure. Many patients ask what is the most ideal eye pressure. This is a complicated patient and depends on many personal factors. While the average eye pressure across the population is 15.5mmHg, the ideal eye pressure for each patient is different and warrants discussion with one’s doctor.
-
Who is a Glaucoma Suspect?
Any individual who has findings that are suspicious for glaucoma without definite signs of glaucoma damage. Often this means the patient may have optic nerve characteristics suggestive of glaucoma but does not have corresponding changes on visual field testing. Depending on the degree of suspicion, glaucoma suspects may be monitored carefully with routine testing and exams or treated.
SYMPTOMS & DIAGNOSIS OF GLAUCOMA
-
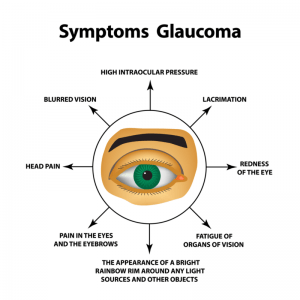
What are the Symptoms of Glaucoma?
For most people with glaucoma, there are no warning signs or noticeable changes in vision until the disease has silently and gradually worsened to a severe stage. About half of those with glaucoma do not yet know they have it. This is why glaucoma is often called the “thief of sight” and one of the main reasons why it is still one of the leading causes of blindness in the world.
In the early stages, glaucoma typically affects peripheral (or side) vision. A common misconception is that those with glaucoma get tunnel vision. Tunnel vision is almost never the way patients experience their glaucoma. Instead, vision changes start with a very subtle blurring which usually begins near the nose. Since we see with both eyes at the same time, vision loss in one eye is often covered up and hidden by the other eye. If left untreated, areas of vision loss will slowly spread and may go unnoticed until it reaches the central vision.
-
When Should Glaucoma Screenings Start?
Glaucoma can affect anybody, which is why regular screenings are important. Because the symptoms of glaucoma can be mild, or even non-existent, it is recommended that individuals get a baseline screening at the age of 40. Some factors suggest a higher risk and may require earlier or more frequent screening, including:
- Those who have a family history of glaucoma;
- Those who are of African American, Latino, or Asian descent;
- Those who are significantly near-sighted;
- Those who have risk factors based on an eye exam, such as elevated eye pressure, narrow angles, or particular optic nerve findings.
How often a glaucoma screening exam should be performed will be determined by the results of your initial exam.
-
What Should I Expect at an Appointment with a Glaucoma Specialist?
The best way to test for glaucoma is through a comprehensive eye exam with an ophthalmologist which includes evaluation of your angle (gonioscopy), and your optic nerve with dilation if appropriate. Additionally, a visual field test and optic nerve photograph or analysis may also be performed.
-
What Is a Visual Field Test?
The primary function of the visual field test is to measure the patient’s peripheral (side) and central vision. This test can find areas of vision loss that may not be noticeable to the patients on their own. During the test, lights of varying brightness appear in different parts of the machine while the patient’s eye is focused on a central spot. The patient clicks a button with each light that they see. The results are compared to the test results of people of a similar age. Results are also compared to prior results from the same patient. The test is repeated to check for possible changes over time.
-
Once Diagnosed, How Often Should I See My Doctor for Glaucoma?
This varies based on the type and degree of glaucoma you have. This may range from every 3 months to every year in stable patients or more often if there are concerning findings.
GLAUCOMA TREATMENT
-
What Are the Surgical Treatments for Glaucoma? What is Minimally Invasive Glaucoma Surgery?
The type of surgery that is best suited for a particular patient is based on many factors such as the type of glaucoma, eye pressure goal, shape of the eye, and prior eye surgeries, amongst other factors. Therefore, it is best to discuss whether you are a candidate for a particular type of surgery with your doctor.
-
What Are the Side Effects of Glaucoma Eye Drops?
Side effects vary amongst drops and can range from irritation, redness, burning, and blurry vision to more general symptoms such as shortness of breath, low blood pressure, fatigue, dizziness, sleep disturbance, and change in taste.
-
What Are Some Alternative Medical Therapies?
There is not strong enough evidence to support alternative therapies for glaucoma, although we are hopeful for the future. Currently, all treatments center around lowering eye pressure to decrease the risk of glaucoma onset or glaucoma progression.
-
How Can I Improve My Vision If I Have Glaucoma?
Currently, there are no methods to reverse vision loss from glaucoma. However, it may be beneficial to see a low-vision specialist. Low-vision specialists can help patients make the most of their vision by employing additional tools or techniques
-
Is Glaucoma Reversible?
Unfortunately, vision loss from glaucoma is not reversible. Therefore, it is important to prevent blindness by diagnosing and treating glaucoma as aggressively as possible early on.


